Rosa Emilia Moraes, Scientific journalist at Linceu Editorial, São José dos Campos, SP, Brazil.
 Prostate cancer is one of the types with the highest incidence and high mortality rate. But except for the risk factors already consolidated by the medical literature as predispositions for the development of the disease (gender, age, race and family health history) the etiology of prostate cancer is still not widely understood (SADRI, et al., 2020).
Prostate cancer is one of the types with the highest incidence and high mortality rate. But except for the risk factors already consolidated by the medical literature as predispositions for the development of the disease (gender, age, race and family health history) the etiology of prostate cancer is still not widely understood (SADRI, et al., 2020).
Studies indicate that infections are potential triggers for carcinogenesis, and that it is plausible that prostatitis is related to the occurrence of cancer. However, Langston et al. (2019) considered that such evidence may have a certain statistical bias, since men without clinical symptoms of the infection are less likely to undergo an examination.
Clinical investigation conducted from December 2018 to January 2021 by the Department of Medicine of the Federal University of Amapá sought to deepen the understanding of the possible relationship between human papillomavirus (HPV) and prostate cancer. The article Presence of HPV in prostate tissue from patients submitted to prostate biopsy was published in the journal of Acta Cirúrgica Brasileira, vol. 37, n 12, as an analytical prospective study in which samples of prostate tissue from 162 patients were collected through biopsy guided by transrectal USG.
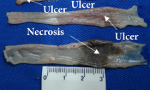
The indication for the procedure was given after the urologists responsible for the patients noticed changes in the prostate that could suggest neoplasia. The samples were placed in an RNA stabilization reagent (RNAlater) and conserved at low temperatures, in order to obtain the best possible quality of genetic material and ensure more accurate results.
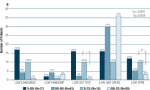
Information about the protocol followed for the q-PCR test for the detection and identification of HPV, and the relationship between the presence of the virus and the confirmation of prostate cancer are displayed in tables that facilitate the understanding of the authors’ conclusion, demonstrating that the distribution of presence of HPV among patients is not necessarily related to the diagnosis of cancer.
After performing all tests, prostate cancer was confirmed in 95 (60.5%) patients, cancer was excluded in 55 (35%) and results were inconclusive in 7 (4.5%). Among those who had the neoplasia confirmed, only 7.4% tested positive for HPV. In cancer-free patients, the percentage of those infected by the virus was 3.6% and among those who presented inconclusive results for the diagnosis of cancer, the presence of HPV infection was not identified.
Thus, the authors could infer that there was no significant difference observed that would clearly demonstrate a relationship between the papillomavirus and prostate cancer. Understanding this dynamic is of substantial relevance in preventing the disease, since there are known and available vaccines against the HPV virus that prevent infection and its adverse effects, such as tumor formation and oncogenesis.
References
LANGSTON, M.E, et al. A systematic review and meta-analysis of associations between clinical prostatitis and prostate cancer: new estimates accounting for detection bias. Cancer Epidemiol Biomarkers Prev [online]. 2019, vol. 28, no. 10, pp. 1594-603 [viewed 28 February 2023]. https://doi.org/10.1158/1055-9965.epi-19-0387. Available from: https://aacrjournals.org/cebp/article/28/10/1594/71744/A-Systematic-Review-and-Meta-analysis-of
NAHAND, J.S., et al. The assessment of a possible link between HPV-mediated inflammation, apoptosis, and angiogenesis in Prostate cancer. Int Immunopharmacol [online]. 2020, vol. 88, 106913 [viewed 28 February 2023]. https://doi.org/10.1016/j.intimp.2020.106913. Available from: https://www.sciencedirect.com/science/article/pii/S156757692032419X
To read the article, access
PEREIRA, N.M., et al. Presence of HPV in prostate tissue from patients submitted to prostate biopsy. Acta Bras Cir [online]. 2022, vol. 37, no. 12, e371205 [viewed 28 February 2023]. https://doi.org/10.1590/acb371205. Available from: https://www.scielo.br/j/acb/a/4bydcD3bqf9sTpmrWMG9Frc/
External links
Acta Cirurgica Brasileira – ACB: https://www.scielo.br/acb/
Universidade Federal do Amapá – Departamento de Medicina: https://www2.unifap.br/medicina/
Acta Cirúrgica Brasileira – Redes Sociais: Facebook | Twitter | Instagram | LinkedIn
Como citar este post [ISO 690/2010]:














Recent Comments