Daniela Barros, postgraduate student of the Surgical Clinic Program at Ribeirão Preto Medical School, University of São Paulo (FMRP-USP). Ribeirão Preto, SP, Brasil.
 Hypocalcemia is the commonest postoperative (PO) complication seen in total thyroidectomy (TT). The main cause of postsurgical (PO) hypocalcemia in TT is hypoparathyroidism, associated to direct injury or devascularization of the parathyroids in the intraoperative period (EDAFE, O., et al.). PO hypocalcemia leads to higher risks for the patient, hospital stay, and costs (NOURELDINE, S.I., et al.).
Hypocalcemia is the commonest postoperative (PO) complication seen in total thyroidectomy (TT). The main cause of postsurgical (PO) hypocalcemia in TT is hypoparathyroidism, associated to direct injury or devascularization of the parathyroids in the intraoperative period (EDAFE, O., et al.). PO hypocalcemia leads to higher risks for the patient, hospital stay, and costs (NOURELDINE, S.I., et al.).
Most studies have used post-surgery serum levels of parathyroid hormone (PTH) and/or Calcium (Ca) as predictors of hypocalcemia or the need for Ca replacement (FILHO, E.B.Y., et al., PUZZIELLO, A., et al.). PTH has been the preferred marker as it presents higher accuracy and faster drops after surgery, even in the first three hours PO. Although the value of using PTH is established, there is still no consensus on the ideal time to collect the hormone, whether during or after surgery and how long after PO (MAZOTAS, I.G., et al.).
Magnesium (Mg) is absorbed in the intestine and actively and passively reabsorbed in the kidney, as maintaining adequate plasma concentrations of the element is necessary for normal PTH secretion (ALLGROVE, J., et al.). The association between hypomagnesemia and the occurrence of PO hypocalcemia in TT have been documented (NELLIS, J.C., et al., LIU, R.H., et al.). In this sense, the possibility of using Mg as a hypocalcemia predictor has some advantages over PTH, such as lower cost and a much narrower band for normal plasma level in that small variations in its concentration could be sufficient to predict the need for Ca replacement (ALLGROVE, J., et al.).
The main objective of the present trial was to assess the ability of serum Mg concentration, measured on the first PO day, to predict the need for Ca replacement in patients undergoing total and completion thyroidectomy. It was identified that in patients undergoing TT, serum Mg1PO was the isolated predictor for the need for Ca replacement (SOARES, C.S.P, et al.).
The paper named Postoperative serum magnesium levels as a predictor for the need for calcium replacement after total thyroidectomy: a prospective study was a collaboration between Brazilian researchers from Universidade Estadual Paulista, Faculdade de Medicina de Botucatu (FMB/UNESP) and A. C. Camargo Cancer Center. Eighty patients undergoing TT, with Mg1PO and PTH dosage in the first (PTH1h) and eighth (PTH8h) hours after TT, were evaluated for the need for Ca replacement. Data were evaluated by uni/multivariate logistic regression and Receiver Operating Characteristic (ROC) curve (SOARES, C.S.P, et al.).
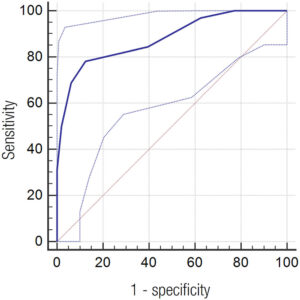
Figure 1. Receiver Operating Characteristic (ROC) curve for the magnesium concentration in the first postoperative day as a predictor of the need for calcium replacement. Area under the ROC curve = 0.88 (95% confidence interval: 0.78 to 0.94, p < 0.0001).
The results showed that 32 patients (40%) required Ca replacement. Median PTH1h, PTH8h and Mg1PO were higher in the no replacement group: 17 versus (vs) 3 pg/mL (p < 0.001), 18.2 vs. 3.0 pg/mL (p < 0.001) and 2 vs 1.6 mg/dL (p < 0.001), respectively. Mg1PO was the isolated predictor for this replacement (odds ratio = 0.0004, 95% confidence interval: 0.000003-0.04; p = 0.001), with the cut-off value of 1.8 mg/dL showing sensitivity and specificity of 78.1% and 87.5%, respectively. Area under the ROC curve for Mg1PO as a predictor of the need for Ca replacement was 0.88 (95% CI: 0.78 to 0.94; p < 0.0001; Figure 1) and the best S and E cut-off point was 1.8 mg/dL. S, E, PPV, NPV and A for this concentration were 78.1%, 87.5%, 80.6%, 85.7% and 83.7%, respectively. (SOARES, C.S.P, et al.).
In recent years, interest has increased in the relationship between the Mg ion and fluctuations in the Ca ion and PTH after thyroid gland removal. Garrahy and cols. retrospectively evaluated 201 thyroidectomy patients from a prospective database and concluded that hypomagnesemia was significantly associated with hypocalcemia and hypoparathyroidism after thyroidectomy (GARRAHY, A., et al.). Brophy and cols. retrospectively evaluated 173 TT patients with Mg measurements from the 1st and 2nd days PO; they concluded that there was a drop in levels of this ion in these two moments and that its concentration on the 2nd day PO was very strongly related to hypocalcemia (BROPHY, C., et al.). Other retrospective studies with larger numbers of patients also reported that hypomagnesemia was significantly associated with postoperative hypocalcemia (NELLIS, J.C. et al., LIU, R.H., et al.).
Despite recent advances to elucidate the complex inter-relationship between the calcemia and magnesemia balance and serum PTH concentration, until now no consensus has been reached from a molecular perspective, as to what the relationship is between falls in Mg and Ca, secondary to a fall in PTH from parathyroid gland injury during thyroidectomy (SOARES, C.S.P, et al.).
This study has merit by demonstrating that the level of serum Mg collected on the first day after surgery presented good sensitivity and specificity in predicting which patients required Ca replacement. Thus, the Mg measurement on the first PO day works as a complementary screening tool, in addition to the already known PTH dosage, to help in the detection of patients that can be safely discharged from the hospital, as they did not require Ca replacement from those who should remain in hospital with monitoring and Ca replacement. Routine use of a single Mg measurement on the first day PO as a marker for Ca replacement after TT has several advantages. The first would be the costs: in our institution, for example, measuring serum Mg is five times less expensive than measuring serum PTH. (SOARES, C.S.P, et al.).
One limitation of this study was the relatively low sample number of 80 patients. We believe that an increased number of evaluated cases could have led to the inclusion of factors such as postoperative serum PTH level as a predictor for replacement. Also, failure to measure preoperative serum Mg could be considered another limitation. If this had been done, it could have clarified whether the postoperative drop in this ion was related to the need for Ca replacement (SOARES, C.S.P, et al.).
In conclusion, serum Mg concentrations collected on the first day after TT, are predictors of the need for Ca replacement, making it an excellent additional tool to screen patients for much earlier hospital discharge after these operations. (SOARES, C.S.P, et al.).
References
ALLGROVE, J., et al. Calcium and Bone Disorders in Children and Adolescents. 2nd, revised edition. Basel: Karger, 2015.
BROPHY, C., et al. Perioperative magnesium levels in total thyroidectomy and relationship to hypocalcemia. Head Neck [online]. 2019, vol. 41, no. 6, pp. 1713-1718 [viewed 19 July 2023]. https://doi.org/10.1002/hed.25644. Available from: https://pubmed.ncbi.nlm.nih.gov/30628752/
EDAFE, O., et al. Systematic review and meta-analysis of predictors of post-thyroidectomy hypocalcaemia. Br J Surg [online]. 2014, vol. 101, no. 4, pp. 307-320 [viewed 19 July 2023]. https://doi.org/10.1371/journal.pone.0207088. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6226183/
GARRAHY, A., et al. Impact of postoperative magnesium levels on early hypocalcemia and permanent hypoparathyroidism after thyroidectomy. Head Neck [online]. 2016, vol. 38, no. 4, pp. 613-619 [viewed 19 July 2023]. https://doi.org/10.1002/hed.23937. Available from: https://pubmed.ncbi.nlm.nih.gov/25491348/
LIU, R.H., et al. Association of Hypocalcemia and Magnesium Disorders With Thyroidectomy in Commercially Insured Patients. JAMA Otolaryngol Head Neck Surg [online]. 2020, vol. 146, no. 3, pp. 237-246 [viewed 19 July 2023]. https://doi.org/10.1001/jamaoto.2019.4193. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6990795/
MAZOTAS, I.G., et al. The role and timing of parathyroid hormone determination after total thyroidectomy. Gland Surg [online]. 2017, vol. 6, suppl. 1, pp. S38-S48 [viewed 19 July 2023]. https://doi.org/10.21037/gs.2017.09.06. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5756748/
NELLIS, J.C., et al. Association between Magnesium Disorders and Hypocalcemia following Thyroidectomy. Otolaryngol Head Neck Surg [online]. 2016, vol. 155, no. 3, pp. 402-410 [viewed 19 July 2023]. https://doi.org/10.1177/0194599816644594. Available from: https://pubmed.ncbi.nlm.nih.gov/27118818/
NOURELDINE, S.I., et al. Early predictors of hypocalcemia after total thyroidectomy: an analysis of 304 patients using a short-stay monitoring protocol. JAMA Otolaryngol Head Neck Surg [online]. 2014, vol. 140, no. 11, pp. 1006-1013 [viewed 19 July 2023]. https://doi.org/10.1001/jamaoto.2014.2435. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4316663/
PUZZIELLO, A., et al. Hypocalcaemia after total thyroidectomy: could intact parathyroid hormone be a predictive factor for transient postoperative hypocalcemia? Surgery [online]. 2015, vol. 157, no. 2, pp. 344-348 [viewed 19 July 2023]. https://doi.org/10.1016/j.surg.2014.09.004. Available from: https://pubmed.ncbi.nlm.nih.gov/25616948/
YUNES FILHO, E.B., et al. The timing of parathyroid hormone measurement defines the cut-off values to accurately predict postoperative hypocalcemia: a prospective study. Endocrine [online]. 2018, vol. 61, no. 2, pp. 224-231 [viewed 19 July 2023]. https://doi.org/10.1007/s12020-018-1601-9. Available from: https://pubmed.ncbi.nlm.nih.gov/29721800/
To read the article, access
SOARES, C.S.P, et al. Postoperative serum magnesium levels as a predictor for the need for calcium replacement after total thyroidectomy: a prospective study. Arch Endocrinol Metab [online]. 2023, vol. 67, no. 3, pp. 355-360 [viewed 19 July 2023]. https://doi.org/10.20945/2359-3997000000581. Available from: https://www.scielo.br/j/aem/a/GwWF3RbPzvG3NrjgmcLxBjB/
External links
Archives of Endocrinology and Metabolism – AEM: https://www.scielo.br/aem
Carlos Segundo Paiva Soares – Orcid: https://orcid.org/0000-0003-0121-9533
Como citar este post [ISO 690/2010]:













Recent Comments