Daniela Barros, post graduate student of the Surgical Clinic Program at Ribeirão Preto Medical School, University of São Paulo (FMRP-USP). Ribeirão Preto, SP, Brasil.
 Osteoporosis is a common disease characterized by low bone strength leading to bone fragility and a consequent susceptibility to fractures (KLIBANSKI, A., et al.). Bone mineral density (BMD) measurement using dual-energy X-ray absorptiometry (DXA) is the standard tool for the diagnosis of osteoporosis.
Osteoporosis is a common disease characterized by low bone strength leading to bone fragility and a consequent susceptibility to fractures (KLIBANSKI, A., et al.). Bone mineral density (BMD) measurement using dual-energy X-ray absorptiometry (DXA) is the standard tool for the diagnosis of osteoporosis.
Investigation of bone microarchitecture and bone remodeling by histomorphometric or micro computed tomography (micro-CT) analysis of the transiliac crest bone biopsy is highly informative (KULAK, CAM., et al.) but it is an invasive procedure or not widely available. Hence, there is a need to develop noninvasive clinically available techniques to evaluate bone quality (PALOMO, T., et al.).
Trabecular bone score (TBS) is an indirect and noninvasive measure of bone quality. A low TBS indicates degraded bone microarchitecture, predicts osteoporotic fracture, and is partially independent of clinical risk factors and BMD (PALOMO, T., et al.).
Image: Unsplash.
In Update on trabecular bone score, article written by PALOMO et al., it was reviewed the current state of TBS, its technical aspects, and its evolving role in the assessment and management of several clinical conditions. The authors worked together in a collaborative manner between Fleury Medicina e Saúde, São Paulo, Brazil, and Unidade de Endocrinologia, Belo Horizonte, Brazil (PALOMO, T., et al.).
There is substantial evidence supporting the use of TBS to assess vertebral, hip, and major osteoporotic fracture risk in postmenopausal women, as well as to assess hip and major osteoporotic fracture risk in men aged > 50 years (PALOMO, T., et al.).
In postmenopausal women, several studies have consistently supported the ability of TBS to predict isolated vertebral or hip, and major osteoporotic fractures (MOF: clinical spine, hip, forearm, and humerus) independently of BMD and CRF (HANS, D., et al.; LESLIE, W.D., et al.; McCLOSKEY, E.V., et al.). On average, every 1-point standard deviation (SD) decline in the TBS leads to a 30%-40% increase in the risk of fragility fractures in postmenopausal women.
TBS complements BMD information and can be used to adjust the FRAX (Fracture Risk Assessment) score to improve risk stratification. While TBS should not be used to monitor antiresorptive therapy, it may be potentially useful for monitoring anabolic therapy (PALOMO, T., et al.). Several cross-sectional and prospective studies including different populations have consistently shown that TBS may improve FRAX accuracy in postmenopausal women and older men (LESLIE, W.D., et al.; McCLOSKEY, E.V., et al.).
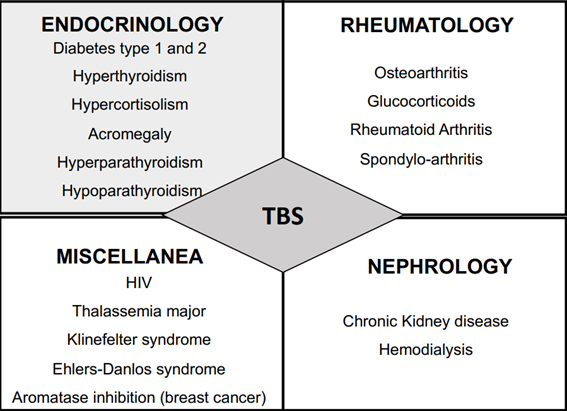
Image: PALOMO, T., et al.
Figure 2. A list of special conditions (causing secondary osteoporosis) known to increase fracture risk in which TBS has been demonstrated to add some clinical value. TBS: Trabecular Bone Score.
There is also a growing body of evidence indicating that TBS is particularly useful as an adjunct to BMD for fracture risk assessment in conditions associated with increased fracture risk, such as type-2 diabetes, chronic corticosteroid excess, and other conditions wherein BMD readings are often misleading (PALOMO, T., et al.). In summary, the relationship between T2D and TBS is mixed. Several studies (DHALIWAL, R., et al.; BONACCORSI, G., et al.), but not all (KIM, J.H., et al.; ZHUKOUSKAYA, V., et al.), have shown that TBS is lower in patients with diabetes, especially in those with poor glycemic control, disease complications, and/or longer duration of disease.
The interference of abdominal soft tissue thickness (STT) on TBS should also be considered when interpreting these findings because image noise can impact TBS evaluation. A new TBS software version based on an algorithm that accounts for STT rather than BMI seems to correct this technical limitation and is under development (PALOMO, T., et al.).
In conclusion, TBS appears to reflect qualitative aspects of skeletal structures that are partially independent of CRFs and DXA BMD measurement, being included as a risk factor in the FRAX tool. However, it should not be used alone to guide clinical decisions, and some limitations, such as the lack of a well-established cutoff point and image noise interference, must be acknowledged. Finally, TBS seems to have a role in anabolic drug response but may not be useful for monitoring antiresorptive therapy (PALOMO, T., et al.).
References
BONACCORSI, G., et al. Comparison of trabecular bone score and hip structural analysis with FRAX® in postmenopausal women with type 2 diabetes mellitus. Aging Clin Exp Res [online]. 2017, vol. 29, no. 5, pp. 951-957 [viewed 21 Dec 2022]. https://doi.org/10.1007/s40520-016-0634-2. Available from: https://pubmed.ncbi.nlm.nih.gov/27722900/
DHALIWAL, R., et al. Bone quality assessment in type 2 diabetes mellitus. Osteoporos Int. 2014, vol. 25, no. 7, pp. 1969-1973 [viewed 21 Dec 2022]. https://doi.org/10.1007/s00198-014-2704-7. Available from: https://pubmed.ncbi.nlm.nih.gov/24718377/
HANS, D., et al. Bone microarchitecture assessed by TBS predicts osteoporotic fractures independent of bone density: The Manitoba study. J Bone Miner Res [online]. 2011, vol. 26, no. 11, pp. 2762-2769 [viewed 21 Dec 2022]. https://doi.org/10.1002/jbmr.499. Available from: https://asbmr.onlinelibrary.wiley.com/doi/full/10.1002/jbmr.499
KIM, J.H., et al. Trabecular bone score as an indicator for skeletal deterioration in diabetes. J Clin Endocrinol Metab [online]. 2015, vol. 100, no. 2, pp. 475-482 [viewed 21 Dec 2022]. https://doi.org/10.1210/jc.2014-2047. Available from: https://pubmed.ncbi.nlm.nih.gov/25368976/
KLIBANSKI, A., et al. Osteoporosis prevention, diagnosis, and therapy. JAMA [online]. 2001, vol. 285, no. 6, pp. 785-95 [viewed 21 December 2022]. https://doi.org/10.1001/jama.285.6.785. Available from: https://jamanetwork.com/journals/jama/article-abstract/193534
KULAK, C.A.M., et al. Bone histomorphometry: A concise review for endocrinologists and clinicians. Arq Bras Endocrinol Metabol [online]. 2010, vol. 54, no. 2, pp. 87-98 [viewed 21 December 2022]. https://doi.org/10.1590/S0004-27302010000200002. Available from: https://www.scielo.br/j/abem/a/y6YzmC97fwFv9TxCSR3xpcS/
LESLIE, W.D., et al. Lumbar spine texture enhances 10-year fracture probability assessment. Osteoporos Int [online]. 2014, vol. 25, no. 9, pp. 2271-2277 [viewed 21 December 2022]. https://doi.org/10.1007/s00198-014-2761-y. Available from: https://link.springer.com/article/10.1007/s00198-014-2761-y
McCLOSKEY E.V., et al. A meta-analysis of trabecular bone score in fracture risk prediction and its relationship to FRAX. J Bone Miner Res [online]. 2016, vol. 31, no. 5, pp. 940-948 [viewed 21 December 2022]. https://doi.org/10.1002/jbmr.2734. Available from: https://pubmed.ncbi.nlm.nih.gov/26498132/
ZHUKOUSKAYA, V., et al. The utility of lumbar spine trabecular bone score and femoral neck bone mineral density for identifying asymptomatic vertebral fractures in well-compensated type 2 diabetic patients. Osteoporos Int [online]. 2016, vol. 27, no. 1, pp. 49-56 [viewed 21 December 2022]. https://doi.org/10.1007/s00198-015-3212-0. Available from: https://pubmed.ncbi.nlm.nih.gov/26138582/
To read the article, access
PALOMO, T., et al. Update on trabecular bone score. Arch Endocrinol Metab. 2022, vol. 66, nº 5, pp.694-706. [viewed 21 Dec 2022]. https://doi.org/10.20945/2359-3997000000559. Available from: https://www.scielo.br/j/aem/a/MtGDBJkn55mpCxTXX7f3Cym/
External links
Archives of Endocrinology and Metabolism – AEM: https://www.scielo.br/aem
Telma Palomo: https://orcid.org/0000-0002-1655-7319
Como citar este post [ISO 690/2010]:


















Recent Comments