Daniela Barros, post graduate student of the Surgical Clinic Program at Ribeirão Preto Medical School, University of São Paulo (FMRP-USP). Ribeirão Preto, SP, Brasil.
 The retrospective study Pregnancy has no significant impact on the prognosis of differentiated thyroid cancer, conducted by Nobre e cols. (NOBRE G.M., et al), included patients diagnosed with differentiated thyroid carcinomas (DTC) before or during pregnancy and treated with standard therapy. Due to the small number of trials addressing these associations, the aim of this study was to evaluate the impact of pregnancy on DTC behavior in a Brazilian cohort of women diagnosed with DTC before or during pregnancy.
The retrospective study Pregnancy has no significant impact on the prognosis of differentiated thyroid cancer, conducted by Nobre e cols. (NOBRE G.M., et al), included patients diagnosed with differentiated thyroid carcinomas (DTC) before or during pregnancy and treated with standard therapy. Due to the small number of trials addressing these associations, the aim of this study was to evaluate the impact of pregnancy on DTC behavior in a Brazilian cohort of women diagnosed with DTC before or during pregnancy.
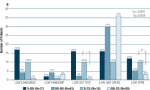
In women diagnosed with DTC before pregnancy, they evaluated the occurrence of progression according to categories of response to therapy based on imaging and non-stimulated thyroglobulin (TG) levels. Of 96 analyzed patients, 76 became pregnant after DTC treatment and 20 were diagnosed with DTC during pregnancy. Among women who became pregnant after a DTC diagnosis, no difference was observed regarding response to therapy before and after pregnancy.
Disease progression after pregnancy was documented in six of these patients, while seven of them presented progression before pregnancy but were only treated after delivery. Patients with DTC diagnosed during pregnancy had a higher rate of distant metastases at diagnosis (30%) compared with the patients who became pregnant after DTC diagnosis (9.2%, p = 0.01). The authors from Rio de Janeiro (RJ, Brazil), reached the conclusion that pregnancy had no impact on the natural course of DTC. Disease progression after pregnancy was limited and probably related to more aggressive disease and higher risk stratification at diagnosis. Still, mild disease progression may have occurred asymptomatically in some patients. (NOBRE G.M., et al)
Pregnancy seems to stimulate the development of existing neoplastic thyroid cells, especially in women with a history of thyroid pathology or genetic predisposition (CABEZÓN, C.A., et al). More than a third of all women diagnosed with thyroid cancer are of childbearing age; thus, the impact of pregnancy on DTC behavior is a pertinent issue (NATIONAL CANCER INSTITUTE).
Many physicians consider the diagnosis of thyroid cancer in women of childbearing age to be challenging, since decisions regarding surgery, radioiodine therapy, and surveillance, must consider the patient’s pregnancy plans. Some authors report a higher frequency of diagnosis of benign and malignant tumors in thyroid nodules detected during pregnancy, with values of up to 80% for all neoplasms, 37%-63% for benign nodules, and 28.5%-43% for DTC (MARLEY, E.F., et al; RAKHLIN, L. et al).

Image: Unsplash
In the present study, the overall cohort had a median age of 27 years (18-40 years) at diagnosis and 32 years (20-44 years) at pregnancy. The median follow-up time was 11 years (1-47 years). In the entire cohort, the initial treatment comprised subtotal (n = 3, 3.1%) or total (n = 93, 96.9%) thyroidectomy followed by radioiodine therapy (n = 71, 73.7%). Among the histological subtypes observed, papillary cancer was the most common (n = 67, 69.8%), followed by the follicular variant of papillary carcinoma (n = 23, 24%), follicular carcinoma (n = 3, 3.1%), and other subtypes (n = 3, 3.1%) including oxyphilic, insular, and tall-cell carcinoma (one case each). The tumors had an initial median size of 2.2 cm (0.3-7.5 cm). At diagnosis, 50 patients had local lymph node metastases (13.5% N1a and 38.5% N1b) and 13 patients (13.5%) had distant metastases, mainly to the lungs (NOBRE G.M., et al).
Among patients who became pregnant after a DTC diagnosis, the responses to therapy prior to the pregnancy were as follows: excellent response, 39.5%; indeterminate response, 18.5%; biochemical incomplete response, 21.0%; and structural incomplete response, 21.0%. The rates of each type of response to therapy were comparable between patients diagnosed with DTC before or during pregnancy (NOBRE G.M., et al).
The results of this study indicate that the impact of pregnancy on DTC appears to be limited. Although it revealed that disease progression occurred in 17.1% of the cases within the first year after delivery, in most cases, the progression was not clinically significant, and most of the affected patients showed only increased TG levels. Most patients had already presented disease progression before pregnancy, and the pregnancy did not seem to have changed their disease status (NOBRE G.M., et al).
Although the DTC had a certain impact on pregnancy in some patients, the morbidity was not increased in these patients compared with other young patients treated at the center where this trial was conducted (VAISMAN, F., et al).
The authors hypothesize that tumors diagnosed during pregnancy could be more responsive to growth stimulation by TSH/β-hCG and were, thus, noticed by palpation during pregnancy. Further studies are required to confirm our findings and determine the potential impact of TSH, β-hCG, and other growth factors on these tumors (NOBRE G.M., et al).
In conclusion, pregnancy has no substantial impact on the natural course of DTC. Rates of recurrence and progression after pregnancy were small and perhaps related to a more aggressive disease and a higher initial risk stratification at diagnosis. Still, disease progression may have occurred asymptomatically in some patients (NOBRE G.M., et al).
Read more
CABEZÓN, C.A., et al. Evolution of differentiated thyroid cancer during pregnancy in a community University Hospital in Buenos Aires, Argentina. Arquivos Brasileiros de Endocrinologia & Metabologia [online]. 2013, vol. 57, no. 4, pp. 307 – 311. [viewed 1 December 2021]. https://doi.org/10.1590/S0004-27302013000400005. Available from: https://www.scielo.br/j/abem/a/ffgcrdqPrHsQgZ6mgChRjXg/?lang=en
MARLEY, E.F., et al. Fine-needle aspiration of thyroid lesions in 57 pregnant and postpartum women. Diagnostic Cytopathology [online]. 1997, vol. 16, no. 2, pp. 122-5 [viewed 1 December 2021]. https://doi.org/10.1002/(sici)1097-0339(199702)16:2%3C122::aid-dc5%3E3.0.co;2-j. Available from: https://pubmed.ncbi.nlm.nih.gov/9067102/
NATIONAL CANCER INSTITUTE. Surveillance, epidemiology, and end results program. 2017. [viewed 1 December 2021]. Available from: www.seer.cancer.gov
RAKHLIN, L. et al. Pregnancy as a Risk Factor for Thyroid Cancer Progression.Current Opinion in Endocrinology, Diabetes and Obesity [online]. 2018, vol. 25, no. 5, pp. 326-9 [viewed 1 December 2021]. https://doi.org/10.1097/med.0000000000000424. Available from: https://pubmed.ncbi.nlm.nih.gov/29965867
VAISMAN, F., et al. Spontaneous Remission in Thyroid Cancer Patients after Biochemical incomplete Response to initial Therapy. Clinical Endocrinology [online]. 2012, vol. 77, no. 1, pp. 132-8 [viewed 1 December 2021]. https://doi.org/10.1111/j.1365-2265.2012.04342.x. Available from: https://pubmed.ncbi.nlm.nih.gov/22248037/
To read the article, access
NOBRE, G.M., et al. Pregnancy has no significant impact on the prognosis of differentiated thyroid cancer. Archives of Endocrinology and Metabolism [online]. 2021, vol. 65, no. 6, pp. 1-10 [viewed 1 December 2021]. https://doi.org/10.20945/2359-3997000000413. Available from: https://www.scielo.br/j/aem/a/DsSnL7HPFMnZntd5SSKckJK/abstract/?lang=en
Link(s)
Gabriela Maia Nobre – Orcid: https://orcid.org/0000-0001-8362-1387
Archives of Endocrinology and Metabolism – AEM: https://www.scielo.br/aem
Como citar este post [ISO 690/2010]:
















Recent Comments