Daniela Barros, post graduate student of the Surgical Clinic Program at Ribeirão Preto Medical School, University of São Paulo (FMRP-USP), Ribeirão Preto, SP, Brazil.
 Currently, congenital hypothyroidism (CH) is a disease with minimal brain involvement and some intellectual and fine motor deficits, and the focus is on ensuring maximum neuromotor and intellectual development of these patients. However, even today, the functioning of a family with a patient with sequelae of CH may be compromised. Diagnosing and correctly treating CH children in a timely (RAMALHO, R.J.R., et al) manner represents a significant benefit for the patient, his or her family, and the community, reducing social, emotional, and financial costs, including higher-cost special schools (ROVET, J.F.).
Currently, congenital hypothyroidism (CH) is a disease with minimal brain involvement and some intellectual and fine motor deficits, and the focus is on ensuring maximum neuromotor and intellectual development of these patients. However, even today, the functioning of a family with a patient with sequelae of CH may be compromised. Diagnosing and correctly treating CH children in a timely (RAMALHO, R.J.R., et al) manner represents a significant benefit for the patient, his or her family, and the community, reducing social, emotional, and financial costs, including higher-cost special schools (ROVET, J.F.).
CH can be permanent (PCH) due to thyroid dysgenesis or dyshormonogenesis or, in up to 35% of cases, transient (TCH) (MESSINA, M.F., et al). Although gene mutations of DUOX2 (a gene that provides instructions for making an enzyme called dual oxidase 2, found in the thyroid gland) and TSH-R have been described in TCH (DE DEKEN, X., et al; FU C., et al; PETERS, C., et al), most of these cases do not have a defined cause, with the iodine intake, the decrease in the cutoff levels of the neo-natal screening programs (NSP), and the time of blood spot collections being the factors initially suggested for the occurrence of nongenetic TCH cases (FORD, G.A., et al).
A neonatal screening program (NSP) for CH (CH- NSP) is one of the most notable milestones in public health, considering the importance of thyroxine in myelination of the infant brain is indisputable, as has been recently shown in magnetic resonance imaging (MRI) studies (ROVET, J.F.). Although the reason to detect severe CH is unequivocal, the benefit for neurodevelopmental outcomes when treating babies with modest TSH elevations and borderline free T4 (FT4) concentrations still generates discussions, with some studies showing a relationship between academic performance and neonatal TSH (LAIN, S.J., et al), while others do not (TRUMPFF, C., et al).
Researchers from Brazil conducted a trial to determinate predictive factors for PCH and verify its prevalence changes over time. Titled Predictive factors for the diagnosis of permanent congenital hypothyroidism and its temporal changes in Sergipe, Brazil – A real-life retrospective study, Gumes-Felix et al assessed the predictive factors for the diagnosis of permanent congenital hypothyroidism in a newborn with abnormal neonatal blood spot TSH. An additional objective is to verify whether the incidence of permanent and transient CH has changed in the periods from 2004 to 2010 and from 2011 to 2015 (GUMES-FELIX, H.M., et al).
The study was conducted at the University Hospital of the Federal University of Sergipe (HU-UFS), the unique entity to perform the NSP in the State of Sergipe (Brazil), which has used the same cutoff point of neonatal bloodspot TSH (5.2 μU/mL) since its implementation. This allows an appropriate comparison of different time periods (RAMALHO, R.J.R., et al; RAMALHO, A.R.O., et al; MATOS, D.M., et al).
In a previous paper, the same authors found that among children with serum initial TSH levels greater than 10 μU/mL (more than two-thirds of the cases had PCH), 13.5% had TCH. In children with initial serum TSH levels greater than 4.2 μU/mL and less than or equal to 10 μU/m, 13.8% had PCH, while 58.1% had TCH (MATOS, D.M., et al).

Image: Freepik.
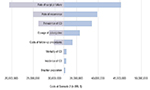
In the present trial, a total of 165 children were evaluated at 3 years of age to verify the diagnosis of PCH. 130 were submitted to a two-step cluster analysis, with the aim of grouping them into homogeneous clusters. The mean incidence of PCH and TCH was calculated from 2004 to 2010 and 2011 to 2015. Sixty-six children were diagnosed with PCH, and 99 were diagnosed with TCH. Eighty-one percent of PCH children and all TCH children with thyroid imaging had glands in situ. Eighty children (61.5%) were in Cluster 1, 8 children (6.2%) were in Cluster 2 and 42 children (32.3%) were in Cluster 3. No children had PCH in Cluster 1, while 87.5% of children in Cluster 2 and all children in Cluster 3 had PCH.
The most important predictor for PCH was the initial serum TSH, which was marginally higher in importance than the blood spot TSH, followed by the initial serum free T4. The mean incidence of PCH and TCH increased over time (GUMES-FELIX, H.M., et al).
Gumes-Felix et al found that while the age of treatment onset and sex were similar in PCH and TCH, the levels of neonatal blood spot and serum initial TSH were higher and the levels of fT4 were lower in PCH than in TCH (GUMES-FELIX, H.M., et al). Most cases of PCH and all cases of TCH had glands in situ. This finding agrees with several previously published reports (RABBIOSI, S., et al; McGRATH, N., et al; LÉGER, J.). The etiology of CH with glands in situ remains unclear, and the factors that determine its clinical diversity are unknown. The possible effects of toxic environmental agents on the fetal and neonatal thyroid gland are currently being studied in several scenarios (LÉGER, J.; McNALLY, R.J.Q., et al; LI, Z.M., et al).
Another important finding of the current work is the significant increase of the incidence of PCH and TCH comparing the 2004-2010 and the 2011-2015 periods in the same region, without demographic changes, with the same iodine intake, the same screening procedure, and the same cutoff point in both periods (MATOS, D.M., et al). A similar increase was also demonstrated in Ireland over a period of 37 years. The authors suggest that other potential causes, such as iodine deficiency or excess, and environmental factors need to be considered (McGRATH, N., et al).
Several pollutants have been studied as potentially toxic to fetal and neonatal thyroid that might impact the transcription of genes involved in thyroid gland development, A Scottish study using space-time clustering suggested the involvement of a spatially varying and transient environmental agent or agents. Such agents could include pollutants or pesticides, which would be expected to occur in more rural communities (McNALLY, R.J.Q., et al).
Brazil is a great consumer of pesticides (MINISTÉRIO DA SAÚDE), but the authors are not aware of any influence of these environmental factors on the incidence of CH in Sergipe. They suggested potential causes of CH, such as iodine deficiency or excess and environmental factors, and genes susceptible to CH (CHEN, J., et al).
The limitations of this study include the possible incomplete quality of medical records, the loss of newborns after neonatal TSH collection and the loss of follow-up before the final diagnosis, which reduced the number of children studied (GUMES-FELIX, H.M., et al).
In conclusion, the two-step cluster analysis discriminated three clusters in children with an altered neonatal TSH blood spot (GUMES-FELIX, H.M., et al).
References
BRASIL. Ministério da Saúde. Pesticides from the perspective of the Brazilian Public Heath. [viewed 2 May 2023]. Brasília: Ministério da Saúde, 2018. Available from: https://bvsms.saude.gov.br/bvs/publicacoes/relatorio_nacional_vigilancia_populacoes_expostas_
agrotoxicos.pdf
CHEN, J., et al. Epidemiologic characteristics, and risk factors for congenital hypothyroidism from 2009 to 2018 in Xiamen, China. Endocr Pract [online]. 2020, vol. 26, no. 6, pp. 585-594 [viewed 2 May 2023]. https://doi.org/10.4158/EP-2019-0491. Available from: https://pubmed.ncbi.nlm.nih.gov/31968198/
DE DEKEN, X., et al. DUOX defects and their roles in congenital hypothyroidism. Methods Mol Biol [online]. 2019, vol. 1982, pp. 667-93 [viewed 2 May 2023]. https://doi.org/10.1007/978-1-4939-9424-3_37. Available from: https://pubmed.ncbi.nlm.nih.gov/31172499/
FORD, G.A., et al. Transient versus Permanent Congenital Hypothyroidism after the Age of 3Years in Infants Detected on the First versus Second Newborn Screening Test in Oregon, USA. Horm Res Paediatr [online]. 2016, vol. 86 no. 3, pp. 169-177 [viewed 2 May 2023]. https://doi.org/10.1159/000448658. Available from: https://pubmed.ncbi.nlm.nih.gov/27595483/
FU, C., et al. Mutation screening of DUOX2 in Chinese patients with congenital hypothyroidism. J Endocrinol Invest [online]. 2015, vol. 38, no. 11, pp. 1219-24. [viewed 2 May 2023]. https://doi.org/10.1007/s40618-015-0382-8. Available from: https://pubmed.ncbi.nlm.nih.gov/26349762/
GUMES-FELIX, H.M., et al. Predictive factors for the diagnosis of permanent congenital hypothyroidism and its temporal changes in Sergipe, Brazil – A real-life retrospective study. Arch Endocrinol Metab [online]. 2023, vol. 67, no. 2, pp. 189-196 [viewed 2 May 2023]. https://doi.org/10.20945/2359-3997000000579. Available from: https://www.scielo.br/j/aem/a/ByspQDPFF7VfSmNzdtB6g3M/
LAIN, S.J., et al. Association between borderline neonatal thyroid-stimulating hormone concentrations and educational and developmental outcomes: a population-based record-linkage study. Lancet Diabetes Endocrinol [online]. 2016, vol. 4, no. 9, pp. 756-765. [viewed 2 May 2023]. https://doi.org/10.1016/S2213-8587(16)30122-X. Available from: https://pubmed.ncbi.nlm.nih.gov/27453174/
LÉGER, J. Épidémiologie de l’hypothyroïdie congénitale en France: données récentes [Epidemiology of congenital hypothyroidism in France: recent data]. Biol Aujourd’hui [online]. 2019, vol. 213, no. 1-2, pp. 1-5 [viewed 2 May 2023]. https://doi.org/10.1051/jbio/2019005. Available from: https://pubmed.ncbi.nlm.nih.gov/31274097/
LI, Z.M., et al. Association of In Utero Persistent Organic Pollutant Exposure with Placental Thyroid Hormones. Endocrinology [online]. 2018, vol. 159, pp. 3473-3481 [viewed 2 May 2023]. https://doi.org/10.1210/en.2018-00542. Available from: https://pubmed.ncbi.nlm.nih.gov/30059991/
MATOS, D.M., et al. Evolution to permanent or transient conditions in children with positive neonatalTSH screening tests in Sergipe, Brazil. Arch Endocrinol Metab [online]. 2016, vol. 60, no. 5, pp. 450-456 [viewed 2 May 2023]. https://doi.org/10.1590/2359-3997000000189. Available from: https://pubmed.ncbi.nlm.nih.gov/27812608/
McGRATH, N., et al. Incidence of Congenital Hypothyroidism Over 37 Years in Ireland. Pediatrics [online]. 2018, vol. 142, no. 4, e20181199 [viewed 2 May 2023]. https://doi.org/10.1542/peds.2018-1199. Available from: https://pubmed.ncbi.nlm.nih.gov/30242075/
McNALLY, R.J.Q., et al. Congenital Hypothyroidism: Space-Time Clustering of Thyroid Dysgenesis Indicates a Role for Environmental Factors in Disease Etiology. Thyroid [online]. 2021, vol. 31, no. 6, pp. 876-883 [viewed 2 May 2023]. https://doi.org/10.1089/thy.2020.0005. Available from: https://pubmed.ncbi.nlm.nih.gov/33183175/
MESSINA, M.F., et al. Early discrimination between transient and permanent congenital hypothyroidism in children with eutopic gland. Horm Res Paediatr [online]. 2015, vol. 84, pp. 159-64 [viewed 2 May 2023]. https://doi.org/10.1159/000435811. Available from: https://pubmed.ncbi.nlm.nih.gov/26160341/
PETERS, C., et al. DUOX2/DUOXA2 mutation frequently cause congenital hypothyroidism that evades detection on newborn screening in the United Kingdom. Thyroid [online]. 2019, vol. 29, no. 6, pp. 790-797 [viewed 2 May 2023]. https://doi.org/10.1089/thy.2018.0587. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6588112/
RABBIOSI, S., et al. Congenital hypothyroidism with eutopic thyroid gland: analysis of clinical and biochemical features at diagnosis and after re-evaluation. J Clin Endocrinol Metab [online]. 2013, vol. 98, no. 4, pp. 1395-402 [viewed 2 May 2023]. https://doi.org/10.1210/jc.2012-3174. Available from: https://pubmed.ncbi.nlm.nih.gov/23426615/
RAMALHO, A.R.O., et al. Programa de triagem neonatal para hipotireoidismo congênito no nordeste do Brasil: critérios diagnósticos e resultados. Arq Bras Endocrinol Metab [online]. 2008, vol. 52, no. 4, pp. 617-27 [viewed 2 May 2023]. https://doi.org/10.1590/s0004-27302008000400007. Available from: https://pubmed.ncbi.nlm.nih.gov/18604374/
RAMALHO, R.J.R., et al. Evolução do programa de triagem neonatal para o hipotireoidismo congênito e fenilcetonúria no Estado de Sergipe de 1995 a 2003. Arq Bras Endocrinol Metab [online]. 2004, vol. 48, no. 6, pp. 890-896 [viewed 2 May 2023]. https://doi.org/10.1590/s0004-27302004000600017. Available from: https://pubmed.ncbi.nlm.nih.gov/15761565/
ROVET, J.F. The role of thyroid hormones for brain development and cognitive function. Endocr Dev [online]. 2014, vol. 26, pp. 26-43 [viewed 2 May 2023]. https://doi.org/10.1159/000363153. Available from: https://pubmed.ncbi.nlm.nih.gov/25231442/
TRUMPFF, C., et al. Thyroid-stimulating hormone (TSH) concentration at birth in Belgian neonates and cognitive development at preschool age. Nutrients [online]. 2015, vol. 7, pp. 9018-9032 [viewed 2 May 2023]. https://10.3390/nu7115450. Available from: https://pubmed.ncbi.nlm.nih.gov/26540070/
To read the article, access
GUMES-FELIX, H.M, et al. Predictive factors for the diagnosis of permanent congenital hypothyroidism and its temporal changes in Sergipe, Brazil – A real-life retrospective study. Arch. Endocrinol. Metab. [online] 2023, vol. 67, no. 2, pp. 189-196 [viewed 2 May 2023]. https://doi.org/10.20945/2359-3997000000579. Available from: https://www.scielo.br/j/aem/a/ByspQDPFF7VfSmNzdtB6g3M/
External links
Archives of Endocrinology and Metabolism – AEM: https://www.scielo.br/aem
Hérika M. Gumes-Felix – Orcid:https://orcid.org/0000-0002-2465-6229
Como citar este post [ISO 690/2010]:















Recent Comments