Daniela Barros, post graduate student of the Surgical Clinic Program at Ribeirão Preto Medical School, University of São Paulo (FMRP-USP). Ribeirão Preto, SP, Brasil.
 From the clinical perspective view, the prognostic role of BRAFV600E mutation is still controversial (SCHEFFEL, R.S., et al.). Several studies were focused on searching for an association between BRAFV600E mutation and features related to an unfavorable course of the disease and showed conflicting results (CZARNIECKA, A. et al; LIU, C. et al and DAMIANI, C. et al). Other trials also have shown an association of mutated BRAFV600E with lymph node metastases, extrathyroidal extension, tumor size, and advanced disease stage (ZHANG, Q. et al).
From the clinical perspective view, the prognostic role of BRAFV600E mutation is still controversial (SCHEFFEL, R.S., et al.). Several studies were focused on searching for an association between BRAFV600E mutation and features related to an unfavorable course of the disease and showed conflicting results (CZARNIECKA, A. et al; LIU, C. et al and DAMIANI, C. et al). Other trials also have shown an association of mutated BRAFV600E with lymph node metastases, extrathyroidal extension, tumor size, and advanced disease stage (ZHANG, Q. et al).
The 2015 American Thyroid Association (ATA) guidelines had included the BRAFV600E mutation status in the stratification system for persistent/recurrent disease according to the “continuum of risk” model. In this proposal, those patients classified as low risk-disease with intrathyroidal PTC lesions of 1-4 cm should be reclassified as intermediate risk if positive BRAFV600E mutation is known (HAUGEN, B.R. et al). However, the impact of the BRAFV600E mutation on the clinical outcomes (persistent disease, recurrence, survival) is not so clear.
In this context, Scheffel et al. aimed to evaluate the impact of the BRAFV600E mutation status on risk stratification as well as on disease outcomes in a cohort of patients with PTC in a tertiary, university-based referral center, in southern Brazil. This study, named “The BRAFV600E mutation analysis and risk stratification in papillary thyroid carcinoma (Arch Endocrinol Metab. [online]. 2020, vol. 64, no. 6, pp. 751-757)”, was a collaboration between researchers from The Federal University of Rio Grande do Sul (Brazil) and Institut de Recherche Interdisciplinaire en Biologie Humaine et Moléculaire, Université Libre de Bruxelles (Belgium).
The subjects included were followed in a cohort of differentiated thyroid cancer (DTC) patients from the Thyroid Outpatient Clinic of the Thyroid Unit, of Hospital de Clínicas de Porto Alegre (HCPA). From 2009 to 2015, all consecutive patients with a histological diagnosis of PTC who had paraffin-embedded tumor tissue available for analysis of the BRAFV600E mutation were included in this study.

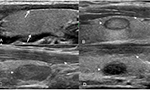
Image: Daniela Barros
The DTC treatment protocol consists of performing total thyroidectomy (TT), followed or not by administration of radioactive iodine (RAI) as indicated, and the use of suppressive levothyroxine therapy according to current guidelines (HAUGEN, B.R. et al). The iodine administration protocol used RAI activities prescribed at the attending physician’s discretion. A post-therapy whole-body scan (WBS) was performed seven to ten days after the RAI administration. The information on BRAFV600E mutation status was not used to decide RAI indication in these patients.
Of the 134 patients evaluated, 44 (32.8%) carried BRAFV600E mutation. The median tumor size was 1.7 cm (P25-75 1.0-3.0), 64 (47.8%) patients had lymph node, and 11 (8.2%) distant metastases. According to the ATA risk stratification system, subjects were classified as low, intermediate, and high risk in 55 (41%), 59 (44%), and 20 (14%) patients, respectively. The data on BRAFV600E mutation reclassified 12 (8.9%) patients from low to intermediate risk. After a median follow-up of 8.5 years, the prevalence of persistent disease was similar in patients with and without BRAFV600E mutation (P = 0.42). Multivariate analysis failed to demonstrate an association between the BRAFV600E mutation and persistent disease status (RR 0.96; 95%CI 0.47-1.94). Notably, none of the patients reclassified from low to intermediate risk showed persistent disease on follow-up. The authors concluded that the inclusion of BRAFV600E mutational status has a limited impact on risk stratification and does not add to the prediction of outcomes in PTC patients.
As mentioned above, the prevalence of positive BRAFV600E mutation was 32.8% in the present study. These numbers are comparable to those reported in previous studies carried out in the Southeastern region of Brazil (28.1 to 48.3%) (17,18), but lower than results obtained from the central (63.8%) and Northeast (65.1%) regions (da SILVA, R.C., et al and PESSÔA-PEREIRA, D., et al.). Indeed, a systematic review of 63 studies (including 20,764 patients) has shown that the prevalence of BRAFV600E mutation varied from 25 to 82.3%. Moreover, when the authors stratified the study subjects into subgroups regarding the ethnicities, they observed a decrease in the heterogeneity of the data (LIU, C. et al.). These results illustrate the heterogeneity of the prevalence of BRAFV600E mutation among the different populations, even in the same genetic background, which could explain (at least in part) the conflicting results of the studies regarding the association of BRAFV600E mutation and outcomes.
Even in the case of a real association of BRAFV600E mutation with disease recurrence, the clinical application of BRAFV600E as a prognostic marker is hampered by its low specificity. Indeed, when the performance of the mutation is analyzed as a diagnostic test for the prediction of recurrent/persistent disease, it has an acceptable sensitivity (60-70%), but poor specificity (34-57%) with a positive predictive positive value of only 7-25% (LIU, C., et al. and ZHANG, Q., et al.). The present study data showed similar results: sensitivity of 45%, a specificity of 69%, and a positive predictive value of 24%.
In conclusion, the inclusion of the BRAFV600E mutation analysis in the risk classification system increases the complexity of care and costs without a clear benefit (HAUGEN, B.R., et al.) BRAFV600E mutation does not seem to be an independent prognostic marker and should be analyzed in association with other prognostic factors.
References
CZARNIECKA, A. et al. BRAF V600E mutation in prognostication of papillary thyroid cancer (PTC) recurrence. Gland Surg. 2016, vol. 5, no 5, pp. 495-505. [viewed 05 January 2021]. https://doi.org/10.21037/gs.2016.09.09. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5106385/
DAMIANI, L. et al. Evaluation of the Role of BRAF V600E Somatic Mutation on Papillary Thyroid Cancer Disease Persistence: A Prospective Study. Eur Thyroid J. 2018, vol. 7 no 5, pp. 251-7. [viewed 05 January 2021]. https://doi.org/10.1159/000490699. Available from: https://pubmed.ncbi.nlm.nih.gov/30374428/
HAUGEN, B. R. et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016, vol. 26, no 1, pp. 1-133. [viewed 05 January 2021]. https://doi.org/10.1089/thy.2015.0020. Available from: https://pubmed.ncbi.nlm.nih.gov/26462967/
LIU, C. et al. Associations between BRAF(V600E) and prognostic factors and poor outcomes in papillary thyroid carcinoma: a meta-analysis. World J Surg Oncol. 2016, vol. 14, no 1, pp.241. [viewed 05 January 2021]. https://doi.org/10.1186/s12957-016-0979-1. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5012084/
PESSÔA-PEREIRA, D. et al. Association between BRAF (V600E) mutation and clinicopathological features of papillary thyroid carcinoma: a Brazilian single-center case series. Arch Endocrinol Metab. 2019, vol 63, no 2, pp. 97-106. [viewed 05 January 2021]. https://doi.org/10.20945/2359-3997000000120. Available from: http://ref.scielo.org/fgv84s
SCHEFFEL, R. S. et al. The long and still uncertain journey of BRAF as a prognostic tool in patients with papillary thyroid cancer. Arch Endocrinol Metab. 2019, vol. 63, no.2, pp. 95-96. [viewed 05 January 2021]. https://doi.org/10.20945/2359-3997000000140. Available from: http://ref.scielo.org/q2pv67
SILVA, R. C. et al. BRAF overexpression is associated with BRAF V600E mutation in papillary thyroid carcinomas. Genet Mol Res.2015, vol. 14, no 2, pp. 5065-75. [viewed 05 January 2021]. https://doi.org/10.4238/2015.May.12.9. Available from: https://pubmed.ncbi.nlm.nih.gov/26125698/
ZHANG, Q. et al. Meta-Analyses of Association Between BRAF(V600E) Mutation and Clinicopathological Features of Papillary Thyroid Carcinoma. Cell Physiol Biochem. 2016, vol. 38, no 2, pp.763-76. [viewed 05 January 2021]. https://doi.org/10.1159/000443032. Available from: https://pubmed.ncbi.nlm.nih.gov/26871894/
To read the articles, acess
SCHEFFEL, R. S. et al. The BRAFV600E mutation analysis and risk stratification in papillary thyroid carcinoma. Arch Endocrinol Metab. [online]. 2020, vol. 64, no. 6, pp. 751-757 [viewed 05 January 2021]. http://dx.doi.org/10.20945/2359-3997000000285. Available from: http://ref.scielo.org/mk49sr
External links
Archives of Endocrinology and Metabolism – AEM: https://www.scielo.br/aem
Rafael Selbach Scheffel: https://orcid.org/0000-0002-8858-309X
Como citar este post [ISO 690/2010]:

















Recent Comments