Daniela Barros, postgraduate student of the Surgical Clinic Program at Ribeirão Preto Medical School, University of São Paulo (FMRP-USP), Ribeirão Preto, SP, Brasil.
 Due to large-scale ultrasound tests performed worldwide, a high number of thyroid nodules are detected, especially nonpalpable ones (INCA, 2021; DEAN, D.S. et al., 2008; PARK, S. et al., 2016). However, just 5%-15% of nodules are diagnosed as cancer (HAUGEN, B.R. et al., 2015). The ultrasound risk stratification system (RSS) has become the cornerstone for selecting nodules for fine needle aspiration (FNA) or follow-up. The nodule rate of malignancy (ROM) is determined by of the presence of suspicious signs, such as solidity, hypoechogenicity, calcifications, irregular margin, taller-than-wide shape, and extra-thyroid extension (HAUGEN, B.R. et al., 2015; NA, D.G. et al., 2016; MOON, W.J., et al., 2011; GHARIB, H. et al., 2016; ROSARIO, P.W. et al., 2013; TESSLER, F.N. et al., 2017).
Due to large-scale ultrasound tests performed worldwide, a high number of thyroid nodules are detected, especially nonpalpable ones (INCA, 2021; DEAN, D.S. et al., 2008; PARK, S. et al., 2016). However, just 5%-15% of nodules are diagnosed as cancer (HAUGEN, B.R. et al., 2015). The ultrasound risk stratification system (RSS) has become the cornerstone for selecting nodules for fine needle aspiration (FNA) or follow-up. The nodule rate of malignancy (ROM) is determined by of the presence of suspicious signs, such as solidity, hypoechogenicity, calcifications, irregular margin, taller-than-wide shape, and extra-thyroid extension (HAUGEN, B.R. et al., 2015; NA, D.G. et al., 2016; MOON, W.J., et al., 2011; GHARIB, H. et al., 2016; ROSARIO, P.W. et al., 2013; TESSLER, F.N. et al., 2017).
One such feature, hypoechogenicity, is the focus of this study, that was designed to determine whether classifying hypoechogenicity in three degrees (mild, moderate, and marked) could improve the distinction between benign and malignant nodules and whether such an approach could influence Category 4 of the Thyroid Imaging Reporting and Data System (TI-RADS).
Conducted by Delfim et al., from the Universidade Federal do Rio de Janeiro, in a collaboration with DASA laboratories, the trial named Does a three-degree hypoechogenicity grading improve ultrasound thyroid nodule risk stratification and affect the TI-RADS 4 category? A retrospective observational study, submitted 2,574 nodules to fine needle aspiration (DELFIM, R.L.C. et al., 2023). They were then classified by the Bethesda System and retrospectively assessed.
Further, a subanalysis considering solid nodules without any additional suspicious findings (n = 565) was performed with the purpose of evaluating mainly TI-RADS 4 nodules. Mild hypoechogenicity was significantly less related to malignancy (odds ratio [OR]: 1.409; CI: 1.086-1.829; p = 0.01), compared to moderate (OR: 4.775; CI: 3.700-6.163; p < 0.001) and marked hypoechogenicity (OR: 8.540; CI: 6.355-11.445; p < 0.001). In addition, mild hypoechogenicity (20.7%) and iso-hyperechogenicity (20.5%) presented a similar rate in the malignant sample. Regarding the subanalysis, no significant association was found between mildly hypoechoic solid nodules and cancer.
The authors concluded that stratifying hypoechogenicity into three degrees influences the confidence in the assessment of the rate of malignancy, indicating that mild hypoechogenicity has a unique low-risk biological behavior that resembles iso-hyperechogenicity, but with minor malignant potential when compared to moderate and marked hypoechogenicity, with special influence on the TI-RADS 4 category (DELFIM, R.L.C. et al., 2023).
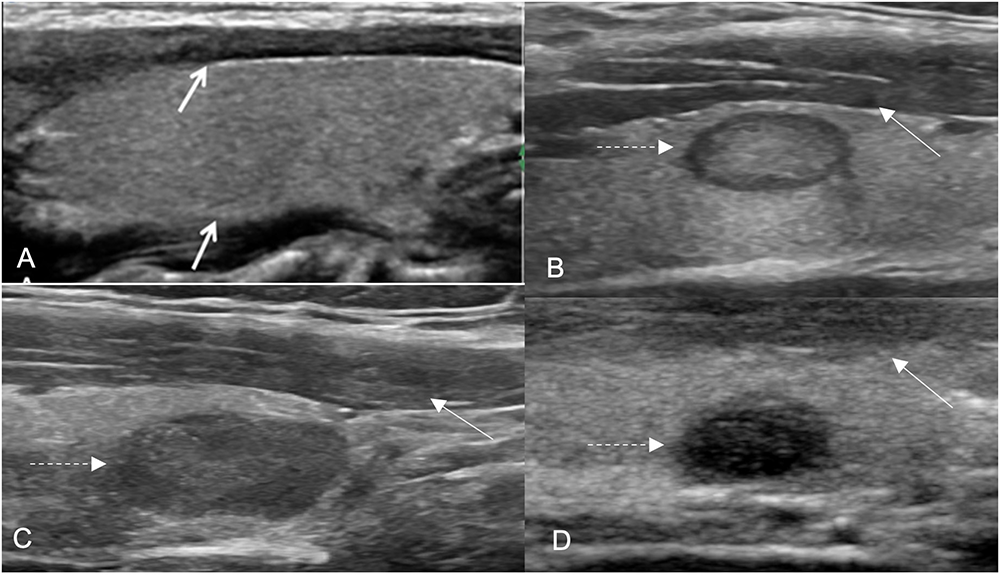
Figure 1. Hypoechoic nodules in different degrees. The nodule hypoechogenicity was compared to that of the anterior strap muscle (ASM) (white arrows).
Discrepancies in grading hypoechogenicity patterns have been reported in previous trials. Some authors have interpreted echogenicity related to the ASM or echogenicity similar to or lower than that of the ASM as marked hypoechogenicity (MOON, W.J. et al., 2011; SHIN, J.H. et al., 2016; LEE, Y.H. et al., 2011). In contrast, ANDERSON, L. et al. classified nodules as mildly, moderately, or very hypoechoic, but in relation to the thyroid parenchyma. Currently, most renowned systems classify hypoechogenicity into two degrees, hypoechogenicity (related to parenchyma) and marked hypoechogenicity, as adopted by the American College of Radiology Thyroid Imaging Reporting and Data System (ACR TI-RADS) (TESSLER, F.N. et al., 2017).
In the current study, an increment in the ROM occurred as the nodules were progressively classified as mildly, moderately, and markedly hypoechoic, as found in the previous study by Delfim et al. (DELFIM, R.L.C. et al., 2017) and reported by Lee and cols. (LEE, J.Y. et al., 2020).
Until nowadays, Delfim et al. was the first group to evaluate the role of three-degree hypoechogenicity grading, comparing it to that of the ASM, in thyroid nodule management (DELFIM, R.L.C. et al., 2017). Additionally, comparing nodule echogenicity to that of the ASM may be advantageous in evaluations performed in the context of lymphocytic thyroiditis (Hashimoto’s thyroiditis), a highly prevalent disorder in which the parenchyma is usually hypoechoic and heterogeneous, which makes it challenging to analyze (ANDERSON, L. et al., 2010; LANGER, J.E. et al., 2011). Hence, this technique is practical and reproducible, and it has no additional costs and can provide greater diagnostic accuracy by conventional ultrasound in predicting malignancy.
In synthesis, conventional ultrasonography is a noninvasive and optimal cost-benefit technique for stratifying thyroid nodules. Albeit most thyroid nodules undergo FNA, the majority have a benign diagnosis. Consequently, improvement on risk stratification is needed.
The key role of a three-degree hypoechogenicity grading system was established according to the present results. Mildly hypoechoic nodules were the most prevalent among hypoechoic nodules, although less associated with malignancy. No association was found between mildly hypoechoic solid nodules and cancer. Moreover, mildly, and moderately hypoechoic nodules are rated together in the TR4 category (TESSLER, F.N. et al., 2017), albeit moderately hypoechoic nodules were the most common among malignant tumors in our study. Therefore, mildly hypoechoic solid nodules should be allocated in a lower risk category (TR4-A) to avoid unnecessary FNA procedures, although further studies are needed to confirm this recommendation (DELFIM, R. L. C. et al., 2023).
References
ANDERSON, L., et al. Hashimoto thyroiditis: Part 1, sonographic analysis of the nodular form of Hashimoto thyroiditis. AJR Am J Roentgenol [online]. 2010, vol. 195, no. 1, pp. 208-215 [viewed 14 September 2023]. https://doi.org/10.2214/AJR.09.2459. Available from: https://pubmed.ncbi.nlm.nih.gov/20566818/
DEAN, D.S., et al. Epidemiology of thyroid nodules. Best Pract Res Clin Endocrinol Metab [online]. 2008, vol. 22, no. 6, pp. 901-911[viewed 14 September 2023]. https://doi.org/10.1016/j.beem.2008.09.019. Available from: https://pubmed.ncbi.nlm.nih.gov/19041821/
DELFIM, R.L.C., et al. Does a three-degree hypoechogenicity grading improve ultrasound thyroid nodule risk stratification and affect the TI-RADS 4 category? A retrospective observational study. Arch. Endocrinol. Metab [online]. 2023, vol. 67, no. 4, e000608 [viewed 14 September 2023]. https://doi.org/10.20945/2359-3997000000608. Available from: https://www.scielo.br/j/aem/a/r4Brm6MzpgWDBxWsPDcWsgk/
DELFIM, R.L.C., et al. Likelihood of malignancy in thyroid nodules according to a proposed Thyroid Imaging Reporting and Data System (TI-RADS) classification merging suspicious and benign ultrasound features. Arch Endocrinol Metab [online]. 2017, vol. 61, no. 3, pp. 211-221 [viewed 14 September 2023]. https://doi.org/10.1590/2359-3997000000262. Available from: https://pubmed.ncbi.nlm.nih.gov/28699990/
GHARIB, H., et al. American association of clinical endocrinologists, american college of endocrinology, and associazione medici endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid nodules – 2016 Update. Endocr Pract [online]. 2016, vol. 22, no. 5, pp. 622-639 [viewed 14 September 2023]. https://doi.org/10.4158/EP161208.GL. Available from: https://pubmed.ncbi.nlm.nih.gov/27167915/
HAUGEN, B.R., et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016, vol. 26, no. 1, pp. 1-133 [viewed 14 September 2023]. https://doi.org/10.1089/thy.2015.0020. Available from: https://pubmed.ncbi.nlm.nih.gov/26462967/
INCA – Instituto Nacional do Câncer José de Alencar Gomes da Silva. Epidemiologia: Nova abordagem para tumor de tireoide. Rede Câncer [online]. 2021, no. 34, pp. 39 [viewed 14 September 2023]. Available from: https://www.inca.gov.br/sites/ufu.sti.inca.local/files//media/document//rrc-34-epidemiologia-nova-abordagem-para-tumor-de-tireoide.pdf
LANGER, J.E., et al. Thyroid nodule sonography: Assessment for risk of malignancy. Imaging Med [online]. 2011, vol. 3, no. 5, pp. 513-524 [viewed 14 September 2023]. Available from: https://www.openaccessjournals.com/articles/thyroid-nodule-sonography-assessment-for-risk-of-malignancy-9177.html
LEE, J.Y., et al. Ultrasound malignancy risk stratification of thyroid nodules based on the degree of hypoechogenicity and echotexture. Eur Radiol [online]. 2020, vol. 30, no. 3, pp. 1653-1663 [viewed 14 September 2023]. https://doi.org/10.1007/s00330-019-06527-8. Available from: https://pubmed.ncbi.nlm.nih.gov/31732777/
LEE, Y.H., et al. Differentiation between benign and malignant solid thyroid nodules using an US classification system. Korean J Radiol [online]. 2011, vol. 12, no. 5, pp. 559-567 [viewed 14 September 2023]. https://doi.org/10.3348/kjr.2011.12.5.559. Available from: https://pubmed.ncbi.nlm.nih.gov/21927557/
MOON, W.J., et al. Ultrasonography and the ultrasound-based management of thyroid nodules: consensus statement and recommendations. Korean J Radiol [online]. 2011, vol. 12, pp. 1-14 [viewed 14 September 2023]. https://doi.org/10.3348/kjr.2011.12.1.1. Available from: https://pubmed.ncbi.nlm.nih.gov/21228935/
NA, D.G., et al. Thyroid Imaging Reporting and Data System Risk Stratification of Thyroid Nodules: Categorization Based on Solidity and Echogenicity. Thyroid [online]. 2016, vol. 26, no. 4, pp. 562-72 [viewed 14 September 2023]. https://doi.org/10.1089/thy.2015.0460. Available from: https://pubmed.ncbi.nlm.nih.gov/26756476/
PARK, S., et al. Association between screening and the thyroid cancer “epidemic” in South Korea: Evidence from a nationwide study. BMJ [online]. 2016, vol. 30, no. 355, pp. i5745 [viewed 14 September 2023]. https://doi.org/10.1136/bmj.i5745. Available from: https://pubmed.ncbi.nlm.nih.gov/27903497/
ROSARIO, P.W., et al. Thyroid nodules and differentiated thyroid cancer: update on the Brazilian consensus. Arq Bras Endocrinol Metabol [online]. 2013, vol. 57, no. 4, pp. 240-64 [viewed 14 September 2023]. https://doi.org.10.1590/s0004-27302013000400002. Available from: https://pubmed.ncbi.nlm.nih.gov/23828432/
SHIN, J.H., et al. Ultrasonography Diagnosis and Imaging-Based Management of Thyroid Nodules: Revised Korean Society of Thyroid Radiology Consensus Statement and Recommendations. Korean J Radiol [online]. 2016, vol. 17, no. 3, pp. 370-95 [viewed 14 September 2023]. https://doi.org/10.3348/kjr.2016.17.3.370. Available from: https://pubmed.ncbi.nlm.nih.gov/27134526/
TESSLER, F.N., et al. ACR Thyroid Imaging, Reporting and Data System (TI-RADS): White Paper of the ACR TI-RADS Committee. J Am Coll Radiol [online]. 2017, vol. 14, no. 5, pp. 587-595 [viewed 14 September 2023]. https://doi.org/10.1016/j.jacr.2017.01.046. Available from: https://pubmed.ncbi.nlm.nih.gov/28372962/
To read the article, access
DELFIM, R.L.C., et al. Does a three-degree hypoechogenicity grading improve ultrasound thyroid nodule risk stratification and affect the TI-RADS 4 category? A retrospective observational study. Arch. Endocrinol. Metab [online]. 2023, vol. 67, no. 4, e000608. [viewed 14 September 2023]. https://doi.org/10.20945/2359-3997000000608. Available from: https://www.scielo.br/j/aem/a/r4Brm6MzpgWDBxWsPDcWsgk/
External links
Archives of Endocrinology and Metabolism – AEM: https://www.scielo.br/aem
Ricardo Luiz Costantin Delfim: https://orcid.org/0000-0002-4026-0187
Como citar este post [ISO 690/2010]:
















Recent Comments